Key Metrics for Measuring the Success of a Clinical Trial
Clinical trials are the backbone of medical advancements, but determining their success goes beyond simply completing the study. Measuring the success of a clinical trial requires analyzing specific metrics that assess its effectiveness, efficiency, and impact. This guide outlines the critical indicators used to measure clinical trial success and highlights their importance in shaping the future of medical research.
Why Metrics Matter in Clinical Trials
Metrics help stakeholders understand the trial’s performance, identify areas for improvement, and ensure that outcomes align with research objectives. These measurements are essential for:
● Ensuring patient safety.
● Validating treatment effectiveness.
● Guiding regulatory approvals.
● Improving the design and execution of future trials.
Key Metrics for Evaluating Clinical Trials
1. Patient Recruitment and Retention Rates
● Recruitment Rate: Tracks how efficiently participants are enrolled within the designated timeline.
● Retention Rate: Measures the percentage of participants who complete the trial.
● Why It Matters: High recruitment and retention rates indicate effective trial design and participant engagement.
2. Adherence to Protocol
● Definition: Measures the extent to which the trial’s procedures are followed as planned.
● Why It Matters: Protocol adherence ensures the reliability and validity of trial outcomes.
3. Timelines and Milestones
● Definition: Tracks whether the trial meets its predefined timelines for key milestones, such as enrollment completion, data collection, and analysis.
● Why It Matters: Staying on track demonstrates efficient project management and resource allocation.
4. Adverse Event Rates
● Definition: Tracks the occurrence and severity of adverse events during the trial.
● Why It Matters: Monitoring adverse events ensures participant safety and informs risk-benefit evaluations.
5. Data Quality and Completeness
● Definition: Assesses the accuracy, consistency, and completeness of collected data.
● Why It Matters: High-quality data are critical for drawing reliable conclusions and advancing treatments.
6. Cost Efficiency
● Definition: Evaluates whether the trial stays within its budget while achieving its objectives.
● Why It Matters: Cost-effective trials maximize resource utilization without compromising outcomes.
7. Regulatory Compliance
● Definition: Measures adherence to regulatory requirements, such as Good Clinical Practice (GCP) and ethical guidelines.
● Why It Matters: Compliance ensures the trial meets legal and ethical obligations, facilitating regulatory approval.
8. Participant Diversity
● Definition: Tracks the representation of diverse demographics, including age, gender, ethnicity, and geography.
● Why It Matters: Diverse trials produce results that are more applicable across populations and address healthcare disparities.
9. Efficacy Outcomes
● Definition: Assesses whether the treatment achieves its intended effect compared to the control or placebo.
● Why It Matters: Demonstrating efficacy is crucial for advancing treatments to the next phase or securing market approval.
10. Stakeholder Satisfaction
● Definition: Gauges the satisfaction of participants, sponsors, and research teams.
● Why It Matters: Positive experiences encourage ongoing participation and investment in clinical research.
Related Posts:
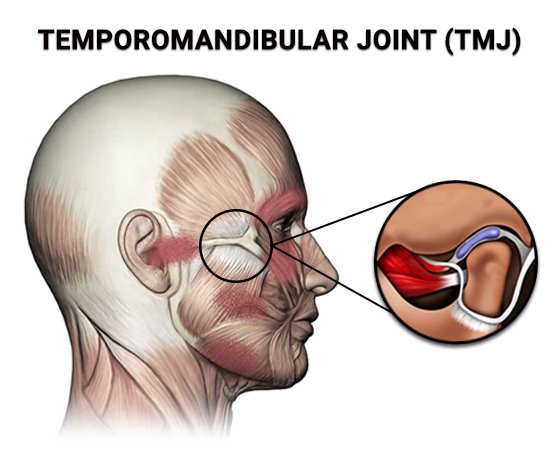
● MRNA Cancer Vaccine Clinical Trials & Research
● Alkeus GLY2 prevents Stargardt Progression in Phase 3 Study
● IO Biotech’s Cancer Vaccine Trial Enrolls Patients with Melanoma and Head/Neck Cancer
Strategies to Improve Metrics
- Enhanced Recruitment Strategies:
○ Use targeted advertising and community outreach to improve enrollment rates.
- Participant-Centric Approaches:
○ Offer flexible scheduling and remote trial options to boost retention.
- Technology Integration:
○ Leverage digital tools, such as wearable devices and eClinical platforms, for real-time data collection and monitoring.
- Training and Communication:
○ Provide ongoing training for research teams and maintain open communication with participants to ensure protocol adherence.
- Data Monitoring:
○ Implement robust data monitoring processes to ensure data accuracy and completeness.
At Clinical Trial Vanguard, we provide resources and insights to help researchers and sponsors measure and improve clinical trial success. By sharing best practices and success stories, we empower stakeholders to achieve their research goals efficiently and ethically.
Measuring the success of a clinical trial requires a comprehensive approach, incorporating metrics that reflect participant engagement, data quality, regulatory compliance, and more. By focusing on these key metrics, researchers can ensure their trials deliver meaningful results that advance medical science.